Everything you need to know are the 3 types of bladder slings and 5 bladder sling complications years later we have described in this article.
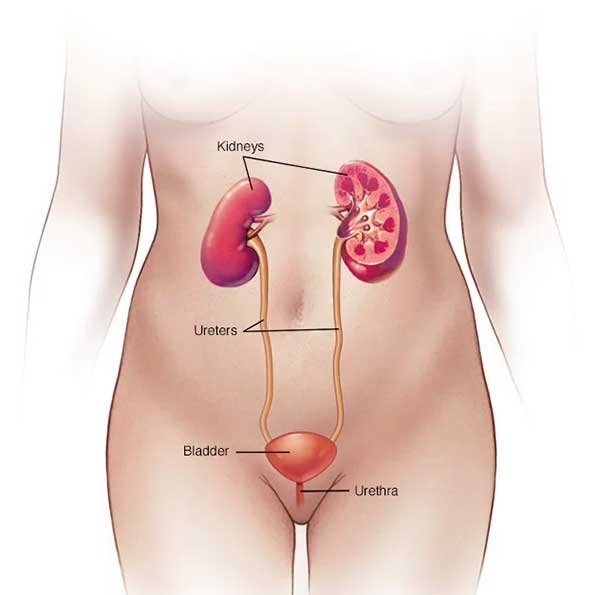
Urinary incontinence is treated by urethral sling surgery, also known as mid-urethral sling surgery. The urethra is wrapped in a sling to help it return to its usual position and to apply pressure on it to improve urine retention. The abdominal (belly) wall is where the sling is fastened.
Muscle, ligament, or tendon tissue from the woman or an animal, such as a pig, can be used to make the sling. It might alternatively be made of a synthetic substance that is compatible with bodily tissues, such as plastic, or an absorbable polymer that degrades over time.

What are bladder sling complications?
Plastic mesh bladder slings are the most prominent type of bladder sling used to treat stress urine incontinence. The majority of women take the surgery well, however, mesh slings have a greater complication risk than tissue slings. Complications might happen right after surgery or years afterward. Some common complications are
- Mesh sling surgery include
- Local irritation at wound site
- Infection
- Vaginal extrusion
- Urinary tract obstruction and urine retention
- Scarring
- Erosion through the urethra
- Contracture
- Pain
- Fistula formation
- Nerve damage
- Inflammation Scar
- Recurrence of incontinence
- Shortness of breath
- Migration of the device
- Swelling and redness at the wound site
- Fatigue
- Vaginal discharge
- Bleeding
3 Types of Bladder Slings
1. Tension-free Sling
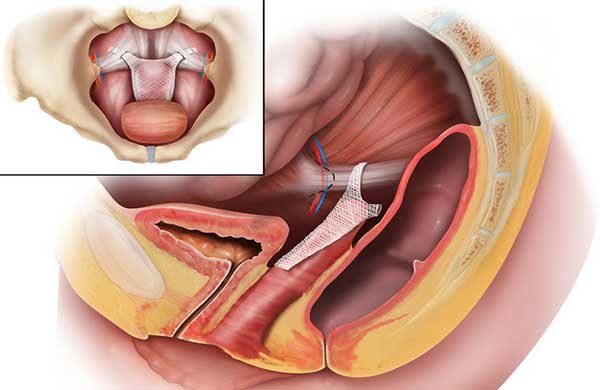
The tension-free sling, which is created from a strip of synthetic mesh tape, is attached without stitching. Instead, the sling is held in place by bodily tissue. Scar tissue builds in and around the mesh over time, preventing it from moving. One of three techniques may be used by your surgeon for a tension-free sling procedure:

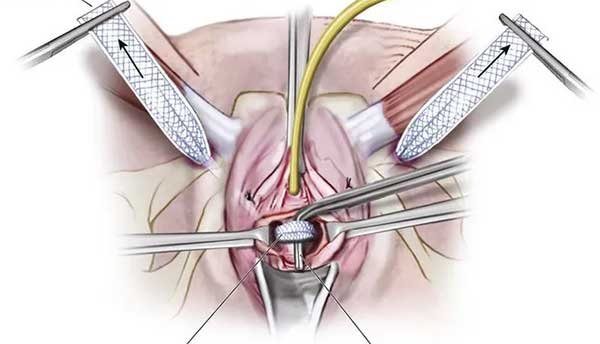
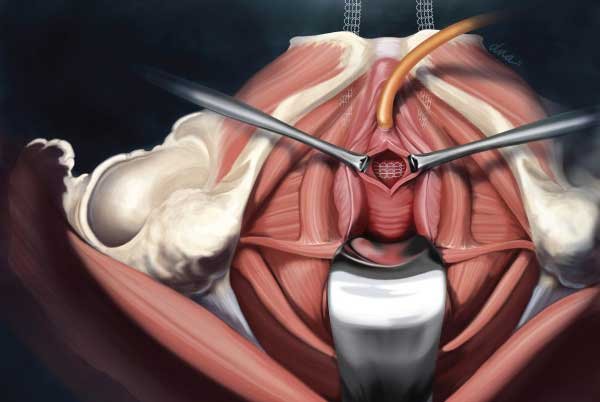
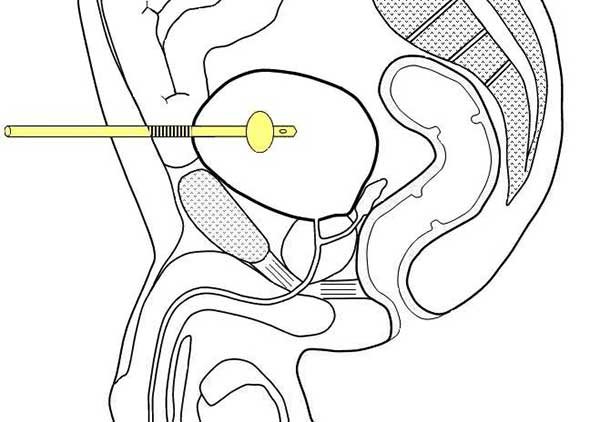
Retropubic. Your surgeon creates a tiny cut (incision) within your vagina right under your urethra with the retropubic approach. Two tiny incisions barely large enough for a needle to pass through are made above your pubic bone by your surgeon. The sling is then passed beneath the urethra and up behind the pubic bone with the use of a needle. The vaginal incision is closed with a few absorbable stitches, and the needle sites can be sealed with skin glue or stitches.
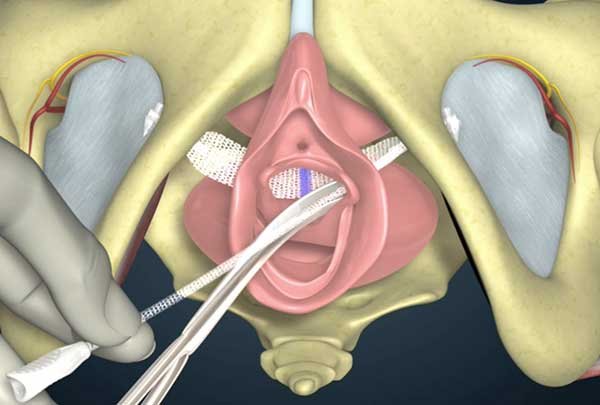
Transobturator: The transobturator method involves a vaginal incision identical to the retropubic approach, as well as a tiny hole on each side of your labia for the needle to pass through. Although the sling follows a different course than the retropubic technique, it is nevertheless put behind the urethra. The vaginal incision is closed with absorbable stitches, and the needle site is closed with skin glue or stitches.
Single-incision Mini: To execute the operation, your surgeon makes only one minor incision in your vaginal wall. Your surgeon will insert the sling through this single incision, similar to the retropubic and transobturator techniques. There are no extra incisions or needle sites required. You may like our recent publication on 20 foods to eat during pregnancy.
The amount of time it takes to recover after tension-free sling surgery varies. Before resuming activities that require heavy lifting or vigorous activity, your doctor may recommend that you rest for two to four weeks. You may have to wait up to six weeks before you may resume sexual activity.
The use of surgical mesh to treat stress urine incontinence can be a safe and effective method. However, significant problems, including material erosion, infection, and discomfort, might develop in certain women.
2. Conventional Sling
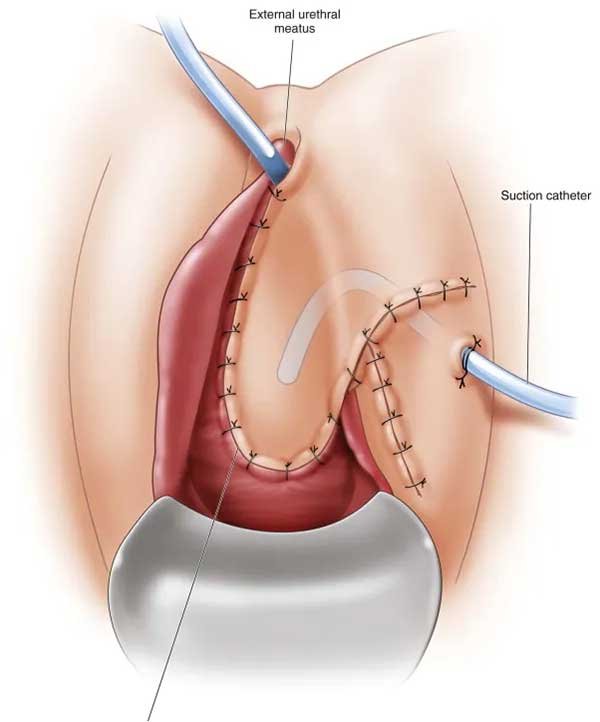
In a traditional procedure, your surgeon creates an incision in your vaginal wall and installs a sling consisting of synthetic mesh tape or potentially your own tissue, tissue from an animal, or tissue from a deceased donor – under the bladder’s neck. Your surgeon pulls the sling to the proper tension and sutures either end of the sling to the pelvic tissue (fascia) or the abdominal wall through another incision in your abdomen.

A tension-free sling may require a bigger incision than a traditional sling. You may require an overnight hospital stay and, in most cases, a lengthier recuperation period. After surgery, you may require a temporary catheter to help you recuperate. Suspension procedures to treat stress incontinence. Procedure to remove the bladder from the neck. Activate the pop-up dialog box.
The urethra and bladder neck are reinforced by a bladder neck suspension, which offers something for the urethra to squeeze against to assist prevent leaking. Your surgeon creates an incision in your lower belly or performs the operation through small incisions with thin equipment and a video camera to execute the treatment (laparoscopic surgery).
Stitches (sutures) are placed in the tissue near the bladder neck by your surgeon. General or spinal anesthesia is required for bladder neck suspension done abdominally. It may be necessary to wear a urinary catheter until you are able to pee normally after a few weeks of recovery. Laparoscopic surgery is likely to take less time to recover from.
3. Nerve Stimulation to Treat Overactive Bladder
Sacral nerve stimulation device implanted. Activate the pop-up dialog box.The nerves that signal the desire to pee are stimulated with tiny electrical impulses in some treatments to treat overactive bladder.
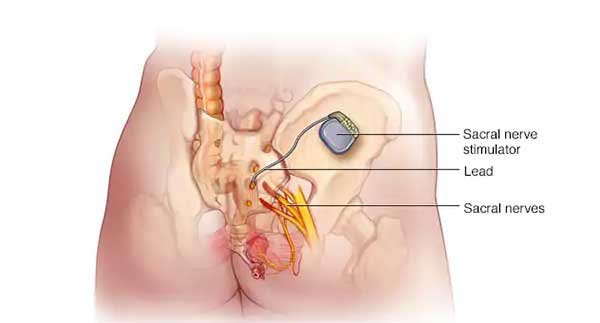
Stimulation of the sacral nerve. A tiny pacemaker-like device is implanted beneath your skin, generally in your buttock. A tiny, electrode-tipped wire attached to the device (stimulator) transmits electrical impulses to the sacral nerve. These painless electrical impulses stop an overactive bladder from sending information to your brain about the desire to pee.
You can attempt sacral nerve stimulation by having a wire implanted under your skin and wearing the stimulator externally. If the stimulator significantly helps your symptoms, you can have it implanted later.
The stimulator is implanted in an operating room under local anesthetic and moderate sedation as an outpatient procedure. With a hand-held programmer, your doctor can alter the degree of stimulation, and you also have control to utilize for modifications.
Stimulation of the tibial nerve. A needle is inserted into the skin around your ankle and electrical stimulation is sent from a nerve in your leg (the tibial nerve) to your spine, where it links with the neurons that regulate your bladder.
Tibial nerve stimulation is done in 12 weekly sessions of around 30 minutes each. Your doctor may prescribe follow-up sessions at regular intervals to sustain the outcomes based on your reaction to the treatment.
Related: 20 foods to avoid during pregnancy
How is bladder sling surgery performed?
Sling operations and bladder neck suspension procedures are the two major types of surgical procedures used to treat stress incontinence. In a sling surgery, your surgeon creates a sling or “hammock” beneath the tube that conducts urine from the bladder (urethra) or the region of thickened muscle where the bladder joins to the urethra using strips of synthetic mesh, your own tissue, or occasionally animal or donor tissue (bladder neck).
The urethra is supported by the sling, which helps maintain it tight and prevents urine leakage, especially when you cough or sneeze. Your condition will determine which sling treatment is ideal for you. You can make the best decision by discussing the risks and advantages of each type of sling operation with your doctor.

5 Complications Associated with Bladder Sling Procedures
1. Bladder Perforation
One of the most serious risks related to TURBT is bladder perforation. Hemorrhage, TURS, infection, the necessity for urgent open surgery, tumor spilling, peritonitis, and death are all possible outcomes. Extraperitoneal perforation is the most common type of bladder perforation. Although intraperitoneal rupture is possible and typically necessitates surgical repair, this problem may normally be controlled with drainage through a urethral catheter (open or laparoscopic).

The location of bladder wall perforation can help determine whether or not on-table cystography is required at the moment of suspected rupture. A cystogram is required to rule out intraperitoneal extravasation in injuries to the anterior bladder wall, dome, or high posterior wall.
Based on the index of suspicion, distention of the abdomen during resection may require a cystogram or an emergency laparotomy. Without a cystogram, if modest exposed regions of perivesical fat are visible during resection but there is no evident extravesical pocket or plane, fast completion of the treatment and implantation of a large-bore catheter may be adequate.
Patients with extravesical illness following perforation repair performed considerably worse than the rest of the group, according to these researchers. Other studies looking at outcomes following TURBT-related perforation, on the other hand, found no evidence of a rise in extravesical illness or worse outcomes. During extensive resection, careful monitoring of input and outflow irrigant volumes may reveal significant concealed bladder perforations.
Perforation during TURBT appears to have the potential to cause extravesical illness, which has a poor prognosis. It’s uncertain if perforation should warrant the consideration of systemic therapy in order to reduce the danger of soft tissue seeding. In addition, if there is a bladder perforation, perioperative intravesical chemotherapy is not recommended.
The severity of this consequence is heightened by the loss of the documented risk-reduction effect of postoperative intravesical chemotherapy, as well as a possible increase in disease progression due to perforation.
2. Urethral Erosion
Erosion happens when synthetic mesh is extruded into the bladder or urethra lumen in the late postoperative phase. The percentage of urethral erosion ranges from 0.03 percent to 0.8 percent. Filling lower urinary tract symptoms such as urgency and urine frequency, pelvic discomfort, dyspareunia, recurrent urinary tract infections, voiding symptoms, and microscopic hematuria are common in people with bladder or urethral erosion.
Some cases of late diagnosis might be the result of unnoticed urethral or bladder damage during surgery. The calcified mesh may be evident as a permanent bladder stone (Figure-4a). These people might be asymptomatic for months or have simple symptoms that progressively worsen. Urethrocystoscopy confirms the diagnosis of urethral or bladder erosion.
Excessive stress of the sling under the urethra causes gradual atrophy and eventual erosion, resulting in late urethral erosion. Hypoestrogenism, previous vaginal or urethral surgery and pelvic radiation are all factors that affect urethral vitality and may increase the risk of erosion.
Mesh removal and urethral repair are required for treatment. Vaginal surgery is frequently used to remove the whole tumor. In some situations of retropubic slings, laparoscopy may be employed. For minor erosions with little tissue loss and no infection, transvaginal partial removal is recommended.
Voiding dysfunction is prevalent following mesh removal. Only four patients (21%) remained entirely asymptomatic when the mesh was removed, according to Starkman et al. SUI recurred in (42%) of the patients, and only (47%) thought they were entirely dry following surgery.
After removing the transvaginal mesh in 17 cases of urethral erosion, only 35.3 percent of patients had total urine continence (64). After removing the endoscopic mesh, the same investigators found a 57.1 percent continence rate.
These findings might indicate that individuals who had endoscopic therapy had less severe erosion. The simultaneous installation of a new SSS, according to all authors, is not recommended. However, an autologous pubovaginal sling may be explored.
3. Urinary Tract Infection (UTI)
Recurrent UT Is following SSS surgery may be a problem caused by urethral/bladder erosion or restriction of the bladder outflow. According to Anger et al.33.6 percent of patients who had sling surgery developed a UTI during the first three months after surgery, rising to 46.7 percent within the first year.
Other authors have recently observed lower rates ranging from 7.4% to 13%, with no significant difference between the retropubic and transobturator methods. Recurrent UTIs caused by a blocked bladder outlet necessitate surgical intervention, which may include mesh lysis or even urethrolysis. Removal of the deteriorated sling and urethral repair is recommended in situations of erosion.
4. Bladder Outlet Obstruction (BOO)
Patients with recurrent urine retention (more than 4 weeks) or overt signs of incomplete emptying, weak urinary stream, and straining to void may have a bladder outlet blockage. However, a considerable proportion of patients have less obvious symptoms, and diagnosing them typically necessitates a high index of suspicion, which is usually prompted by symptoms like urgency, frequency, and nocturia.
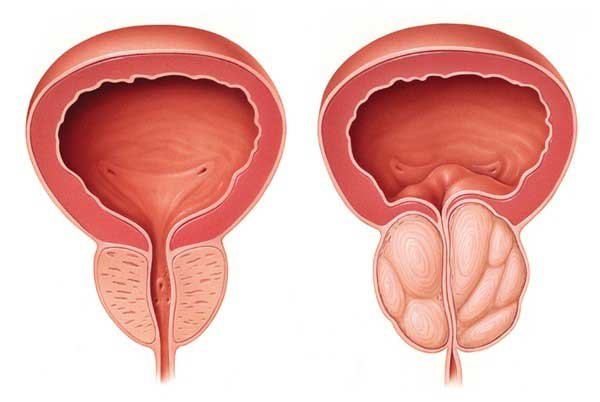
The diagnosis of BOO in women can be difficult, and it should be based on the patient’s medical history, physical examination, lower urinary tract imaging, and urodynamic pressure-flow parameters. Urodynamic observations in a patient with BOO caused by a retropubic SSS, with elevated detrusor pressures (short arrow) and a low maximal flow rate (long arrow).
Because of the probable attachment of the urethra to the pubis and the periurethral fibrotic process, a single mesh transaction may be inadequate to alleviate BOO when outlet blockage is discovered a long time after sling surgery.
In these situations, urethrolysis with mesh transection is advised, with success rates ranging from 70 to 85 percent with SUI recurrence occurring in around 19 percent of cases. If a second urethrolysis is required, the resolution rate is around 92%, with incontinence recurrence rates comparable to those seen after the first one (22%).
5. Surgical Pain
One of the most common consequences of suburethral sling treatments is groin and leg pain. The TOMUS experiment, which compared the transobturator and retropubic procedures and followed 597 patients for a year, found that the retropubic slings had a lower incidence of so-called neurological symptoms 4.0% than the transobturator slings (9.4%). The pain usually goes away during the first few weeks following surgery, although it can last up to four weeks in 1 percent to 2.7 percent of people.

Postoperative discomfort can be caused by a variety of causes, including needle passage through the pelvic muscles, infection, haematoma, and, more rarely, obturator nerve damage, which occurs in less than 1% of patients.
The inflammatory reaction of the sling material may cause tissue retraction and hypertonia of the obturator muscle, simulating a pinched pudendal nerve and causing groin and perineal discomfort, it was suggested.
Treatment should be tailored to the etiological cause and might range from simple analgesics to abscess or haematoma drainage. Sling removal should be considered in situations of severe or chronic infection. Patients who continue to have discomfort despite receiving appropriate conservative therapy may potentially be candidates for sling removal.

What Actions has the FDA taken?
The FDA is still working to improve women’s health and access to safe and effective medical devices. The FDA’s work in the area of urogynecologic surgical mesh has centered on identifying benefit-risk problems with certain of these devices and increasing the FDA’s regulatory control to safeguard patients while allowing those who require these devices to benefit from them.
The FDA’s Ongoing Efforts in the Area of Urogynecologic Surgical Mesh
- Reviewing and interpreting published literature, Medical Device Reports (adverse event reports), and FDA postmarket data.
- Conducting epidemiological study on the safety and effectiveness of surgical mesh for stress urine incontinence (SUI) and pelvic organ prolapse as part of our endeavor to better understand probable adverse events linked with surgical mesh for SUI and POP.
- Working with professional societies and other stakeholders to better understand the postmarket performance of urogynecologic surgical mesh devices, as well as the occurrence of and signs and symptoms associated with specific adverse events, such as low-frequency but life-altering adverse events that can occur after surgical mesh repairs.
Reclassification of the Device
Surgical Instrumentation for Use with Urogynecologic Surgical Mesh received a final reclassification order from the FDA today, moving it from Class I to Class II. Needle passes and trocars, needle guides, fixation tools, and tissue anchors are among the surgical devices covered by the order for treatments such as transvaginal POP repair, sacral colpopexy (transabdominal POP repair), and female SUI therapy.

This should not come as a surprise, nor should it result in a change in the present product lineup. This final order, which was first suggested in May 2014, had been anticipated. It builds on previous FDA decisions to reclassify surgical mesh for transvaginal pelvic organ prolapse (POP) repair from class II to class III devices, and it includes midurethral sling installation equipment.
The FDA and the Gastroenterology-Urology Devices Panel of the Medical Devices Advisory Committee agreed to “up classify” instruments specifically designed for use with urogynecology mesh, based on updated analyses of adverse event (AE) information associated with stress urinary incontinence procedures (retropubic, transobturator, mini-sling) and POP procedures (transvaginal and transabdominal sacral colpopexy).
It builds on previous FDA decisions to categorize transvaginal pelvic organ prolapse (POP) repair surgical mesh from class II to class III devices. The medical literature, the MAUDE, and the Medical Device Reporting (MDR) databases were used to gather AEs. Because of the nature of the AE complaints, it was difficult to attribute them to the surgical mesh or the instruments.
As a consequence, the FDA determined that perioperative adverse events including organ perforation, hemorrhage and bleeding, nerve damage, and discomfort are “induced by or linked to” the use of specialized surgical instruments to insert, implant, fix, or anchor surgical mesh during the Urogynecologic treatment.
Has there Been a Recall of Transvaginal Mesh?
Pelvic organ prolapse (POP) and stress urine incontinence are occasionally treated using transvaginal mesh devices (SUI). Only one transvaginal mesh device has been recalled, despite thousands of claims of catastrophic injury. Several firms, however, have stopped producing their items.
In 1996, the US Food and Drug Administration approved the ProteGen Sling as the first mesh device for SUI. Three years later, Boston Scientific issued a recall for the product. However, the FDA approved numerous other items based on the ProteGen Sling’s concept before the product was taken off the market.
After reclassifying medical devices as “high-risk,” the FDA has issued safety notifications, created advisory groups, and even forced manufacturers to cease selling surgical mesh for specific transvaginal repairs. After encountering problems such as mesh erosion, organ perforation, and infection, more than 100,000 women have launched transvaginal mesh lawsuits against the manufacturers.
Despite the fact that other mesh producers have stopped their goods, they have never filed a recall.
Bladder Mesh Surgery Recovery Time
For one week, you should be quite inactive: no lifting of more than 10 pounds and no intense activities (running, lifting weights, etc.). When picking items up from the floor, try to avoid squatting or leaning over. It’s good to sit in a chair. Although some coughing or sneezing is unavoidable during the first two weeks, try to keep it to a minimum.

It’s important to note that the limits listed above do not inevitably imply “no work.” Depending on the sort of work they perform and how they recover, some patients can return to work within a few days. Increase your regular activities by 2-3 weeks after one week, with the following exceptions: Tampons, douching, and intercourse are not permitted until two weeks following surgery.
Follow the guidelines for the longest duration of inactivity if you’re having another procedure at the same time as the sling.

Minor and Long-Term Complications
Minor problems, including bleeding, urine retention for a short period of time, and post-surgery discomfort, are usually easy to address. Long-term problems including vaginal extrusion, erosion, organ perforation, and recurring infections might make treatment more challenging.
Long-term issues may necessitate revision operations, which can be tough for women. Sepsis, for example, is a life-threatening infection. Some of these issues may arise as a result of surgical procedures.

Vaginal Extrusion and Erosion
The most common documented consequence of transvaginal POP repair with surgical mesh is mesh erosion through the vagina, also known as exposure, extrusion, or protrusion. When transvaginal mesh erodes through tissue and becomes visible, this happens. Erosion may be very painful, and vaginal erosion makes intercourse nearly impossible.
Aside from the vaginal area, erosion can damage a number of other organs. Urinary tract erosion can result in recurrent infections as well as excruciating discomfort. Infections, discomfort, and irregular connections are known as fistulas can result from erosion into the bladder or rectum. Abscesses are another issue induced by mesh degradation.
- Vaginal discharge is a kind of vaginal discharge that occurs when a woman
- Scarring on the vaginal wall

Extrusion Case Study
Dr. Andrew L. Siegel recounts a 48-year-old lady who underwent an ObTape sling operation in case reports published in the journal Urology. Her spouse complained of discomfort during intercourse, and she complained of a continuous yellow vaginal discharge.
Symptoms of Extrusion
Three months following sling surgery, one lady experienced vaginal extrusion. During sexual intercourse, her spouse reported he felt “teeth in her vagina. “Three months after surgery, she said that during sexual intercourse, her husband felt ‘tooth’ in her vagina”, Siegel wrote. Conservative erosion management may be achievable in some instances.
Some surgeons, for example, may prescribe topical estrogen cream to aid in the healing of vaginal tissues. However, the woman had recurrent incontinence and required the removal of the whole sling and replacement with a new one.
Bladder and Bowel Perforation
Only the retropubic approach has been used to describe bowel perforation, a life-threatening condition. With an estimated frequency of 0.03 percent to 0.7 percent, there have been few instances recorded. Previous pelvic surgery is the most significant risk factor since it is thought to enhance the probability of bowel fixation in the retropubic region.
Abdominal discomfort, fever, malaise, leukocytosis, sepsis, and bowel fluid discharge from the surgical site are all possible symptoms. The sling is removed and an exploratory laparotomy is performed to heal the bowel.
In situations of late diagnosis and poor tissue quality, where a primary repair is deemed high risk, a temporary bowel diversion may be necessary. It’s worth noting that because the transobturator procedure avoids the retropubic region, this major problem is almost eliminated.

Perforation Case Study
objective: is to show a series of women who presented late with mid-urethral synthetic slings perforating the bladder and their care. This is an uncommon complication that can cause severe morbidity and have medico-legal ramifications.
Patients and methods: Following the insertion of a synthetic mid-urethral sling, nine ladies with urinary complaints were brought to our center for additional assessment.
The ladies presented between 8 weeks and 18 months after the sling was first placed. Eight patients had tension-free vaginal tape inserted via the retropubic route, and one patient had an I-Stop device-assisted ‘outside-in’ obturator sling (CL Medical, Lyon, France).
Dysuria was reported by six people, recurrent urinary tract infection by four people, frequency and urgency by four people, and pelvic discomfort by two people. On the exposed sling material, seven of the nine women developed bladder calculi, which were all apparent on plain X-ray.
Perforations were seen in more than one location in six women; three had urethral perforation along with anterolateral bladder damage, and the other three had bilateral bladder perforation. Cystoscopy and cystolithopaxy were performed initially, followed by transurethral resection (TUR) of the visible prolene mesh into the detrusor muscle.
To clear all of the mesh, one lady used two TURs. To clear all of the mesh, one lady used two TURs. Two women had further open surgery to remove the residual mesh, both for persistent pelvic discomfort that was relieved following revision surgery.
After tape division/excision, all of the women’s symptoms went away, however, they all developed recurring stress urine incontinence. We employed a unique approach to removing intraurethral mesh by urethral inserting a nasal speculum and excising the tape under direct vision where resection was difficult due to poor endoscopic views, posing a considerable risk of sphincter damage.

Complications During or Shortly After Surgery
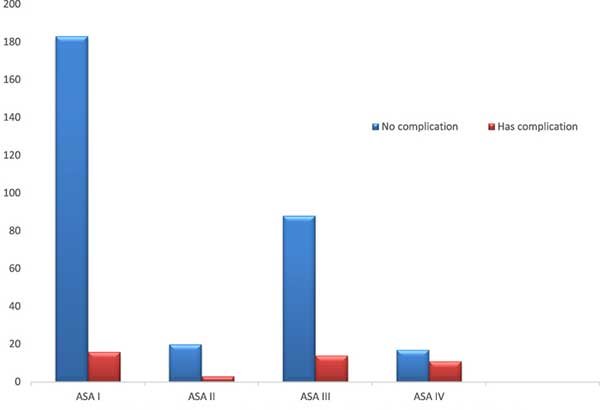
Kim Keltie and colleagues monitored 92,246 women who had transvaginal mesh slings placed for incontinence in a study published in Nature in 2017. The study discovered a 9.8% complication rate within 30 days or five years after the mesh treatment.
According to Rardin, bladder perforation, voiding dysfunction, mesh erosion, and post-operative discomfort are the most prevalent problems after sling treatments.
“Complications can sometimes have a far greater impact than the primary urine incontinence,” Rardin noted. “It’s too critical to bear sling placement difficulties seriously. Let patients know that their symptoms are important and that consequences may be managed.”

Postoperative Complications
Postoperative urinary retention can manifest as suprapubic soreness or discomfort, bladder spasm, and/or urine leaks along with the inability to pee after a surgical treatment. However, anesthetic or sedatives used during the procedure may mask some or all of these symptoms.
Despite having over 600 mL in their bladder, more than 60% of outpatient surgery patients had no subjective symptoms of retention, according to one research. It’s also important to keep track of how long a postoperative patient has gone without voiding. Most people should not spend more than 6 to 7 hours without urinating.
Postoperative Complication Rates
2017 Postoperative Mesh Sling Complications: Average Rates
| Complication | Retropubic Sling | Transobturator Sling |
| Bleeding | 0.7 to 8 percent | 0 to 2 percent |
| Bladder Injury | 0.7 to 24 percent | 0 to 15 percent |
| Urethral Injury | 0.07 to 0.2 percent | 0.1 to 2.5 percent |
| Urethral Erosion | 0.03 to 0.8 percent | 0.03 to 0.8 percent |
| Intestinal Injury | 0.03 to 0.7 percent | 0 percent |
| Vaginal Erosion | 0 to 1.5 percent | 0 to 10.9 percent |
| Urinary Tract Infection | 7.4 to 13 percent | 7.4 to 13 percent |
| Pain | 4 percent | 9.4 percent |
| Urgency urination | 0.2 to 25 percent | 0 to 15.6 percent |
| Bladder obstruction | 6 to 18.3 percent | 3 to 11 percent |
| Urinary retention | 4.0 to 19.5 percent | 2.7 to 11 percent |

Complication Rates by Type of Sling
Urinary incontinence is a significant public-health issue. It is believed that up to one-third of women over the age of 18 in Europe are affected. The frequency rises with age, peaking at 45 percent at 60. Because of its simplicity, speed, and low invasiveness, the tension-free vaginal tape (TVT) method was established in 1995 and has revolutionized the surgical treatment of female stress urinary incontinence (SUI).
Patients, on the other hand, are at risk of a variety of problems. The blind passage of the tape via the retropubic area, which might result in bladder or bowel perforation or vascular damage, is one type of problem. The other group includes voiding problems including dysuria and de novo urgency.

Bladder Sling Complications and Interstitial Cystitis
Interstitial cystitis (IC), a painful bladder ailment that affects millions of Americans, has certain symptoms with bladder sling problems. Women are more prone than males to get the condition. Pelvic and bladder discomfort, painful sexual intercourse, and urine urgency are common indications of IC that may coincide with bladder sling problems.
While a mesh bladder sling may be used to treat urine incontinence, most clinicians treat IC with drugs rather than surgery. However, these drugs have their own set of negative effects.
In the United States, Elmiron (pentosan polysulfate sodium) is the only FDA-approved oral medicine for treating the pain and discomfort of IC. Elmiron has been related to a degenerative visual disorder known as pigmentary maculopathy in recent investigations.
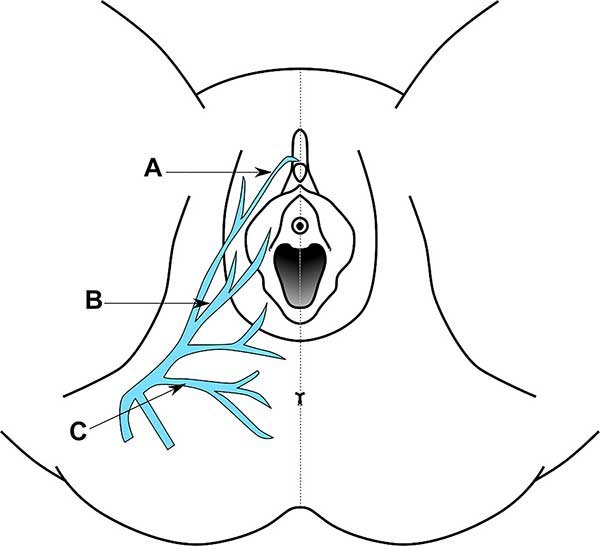
Pudendal Neuralgia
Pudendal Neuralgia is a painful disorder that occurs when the pudendal nerve in the pelvis is compressed, inflamed, or tense. Some patients describe triggering events including childbirth, pelvic surgery or trauma, persistent constipation, or cycling.
Pelvic discomfort or burning, which is worsened by sitting, may be eased by standing, laying down, or sitting on the toilet seat. Perineum sensitivity can be increased or decreased. Pain associated with arousal, intercourse, or orgasm is a sign of sexual dysfunction.
Difficulty or discomfort passing urine or utilizing the bowels, which may lead to bladder or bowel control loss. A sensation of something being inside the vaginal or rectum. Diagnosis entails ruling out other illnesses that might be causing these symptoms, including interstitial cystitis, chronic prostatitis, vulvodynia, and others.
